The Role of Lifestyle Medicine in Menopausal Health: A Deep Dive into the Lifestyle Strategies you can use

Menopause isn’t an illness to fix. It’s a biological transition — a recalibration of your body’s internal systems as estrogen and progesterone naturally decline. These hormonal shifts can bring changes in mood, sleep, weight, and energy, but they also open a powerful opportunity to pause, reflect, and intentionally create the foundation for the next stage of life.
Lifestyle medicine gives us that foundation.
Its six pillars — nutrition, physical activity, mental well-being, avoidance of risky substances, restorative sleep, and healthy relationships — offer evidence-based, practical ways to improve symptoms now while protecting long-term health. In fact, research shows that these lifestyle approaches can reduce the risk of cardiovascular disease, osteoporosis, diabetes, depression, and cognitive decline — all of which become more common after menopause [1].
Menopause can feel like a loss of control, but when you understand how daily habits shape your hormones, metabolism, and mood, it becomes a time to restore calm, rebuild confidence, and take back ownership of your body’s story.
1. Nourishment as Medicine
Why what you eat matters even more now
As estrogen declines, your metabolism slows, muscle mass naturally falls, and fat redistributes toward the abdomen [2]. Blood sugar and cholesterol tend to rise, and inflammation becomes easier to trigger. Food isn’t just fuel — it’s information for your cells. Every meal influences hormone balance, gut bacteria, and the way you metabolise energy.
Mediterranean-style eating
Among all studied diets, the Mediterranean diet stands out for menopausal health. It’s built around colourful plants, whole grains, legumes, olive oil, nuts, and fish — with small amounts of dairy and minimal processed food. Studies show it lowers inflammation, improves mood, and protects against heart disease [3-7].
Women who follow it closely report fewer hot flushes, better energy, and a stronger sense of well-being [6]. Olive oil’s polyphenols, leafy-green antioxidants, and omega-3 fats from fish all help calm the inflammatory pathways that estrogen used to regulate.
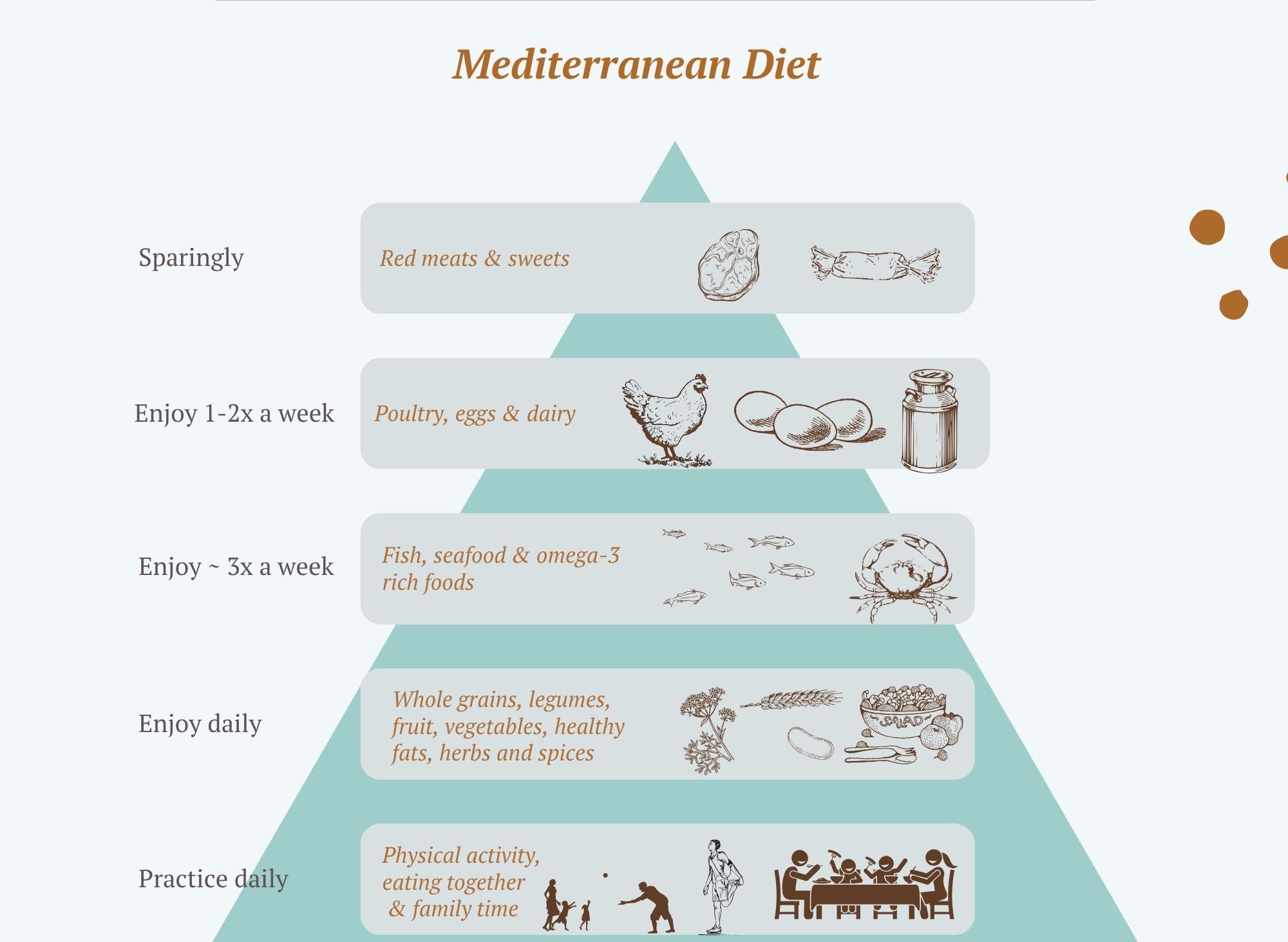
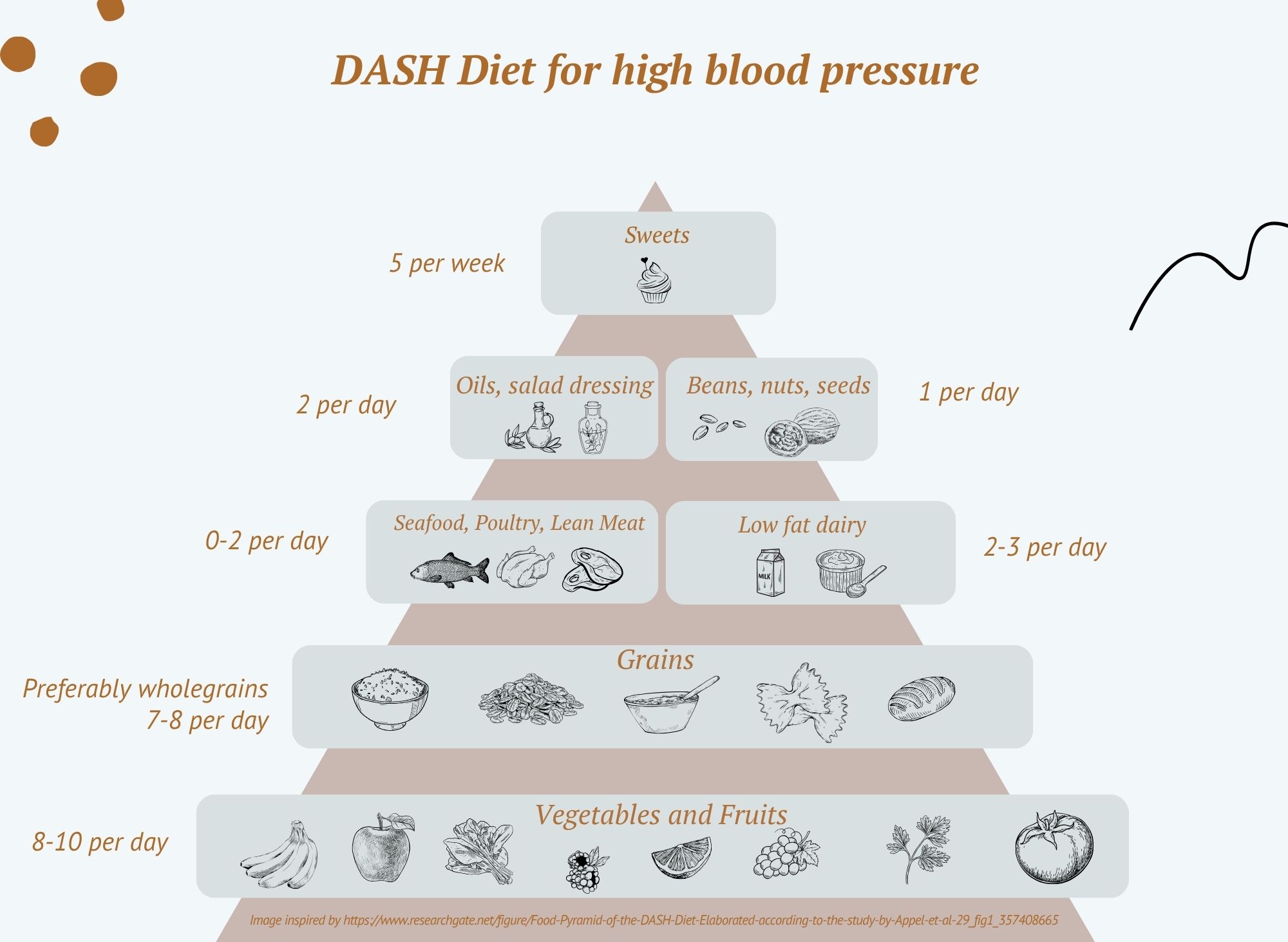
Other patterns that work
The DASH diet (originally designed for blood-pressure control) shares many of the same principles, with an emphasis on potassium-, magnesium-, and calcium-rich foods [8].
Plant-forward or flexitarian diets are also beneficial, improving gut-microbiome diversity and lowering cardiovascular risk [9].
Some women explore intermittent fasting or time-restricted eating to stabilise insulin and appetite. Early data look promising, but long-term studies in midlife women are still limited [10].
Key nutrients for bone, muscle, and mood
-
Calcium 700–1 200 mg/day and vitamin D 800–1 000 IU/day protect bone density [11-12].
-
Protein 1.0–1.2 g/kg body weight daily maintains lean mass and metabolism [13].
-
Magnesium, vitamin K2, and antioxidants from plants further support bone and cardiovascular health.
-
Omega-3 fats from oily fish and walnuts may ease inflammation and mood changes.
Phytoestrogens and soy
Soy contains natural compounds (isoflavones) that gently mimic estrogen. For some women, eating whole soy foods — tofu, tempeh, edamame — can reduce hot-flush frequency and improve cholesterol [14-15]. The response varies between individuals depending on gut bacteria that convert isoflavones to “equol,” their active form.
From evidence to everyday
You don’t need a perfect diet — you need a pattern that nourishes consistently.
Aim to fill half your plate with vegetables, include a protein source at every meal, swap refined grains for whole ones, cook with olive oil, and keep ultra-processed foods for occasional treats. Over time, these small choices re-balance metabolism, support hormones, and stabilise mood and energy.
2. Movement and Muscular Vitality
Why movement becomes medicine in midlife
During the menopausal transition, many women notice body composition changes despite no major change in diet. That’s because estrogen normally supports muscle protein synthesis and mitochondrial efficiency [17]. Without it, muscle mass and metabolic rate fall while body fat rises — particularly around the middle. Movement directly counteracts this.
Aerobic exercise for heart and brain
Activities that raise your heart rate — brisk walking, cycling, swimming, dancing — reduce blood pressure, improve cholesterol, and sharpen cognition [18-21].
Even four moderate sessions a week can lift mood and increase energy [19].
The key is regularity: consistency over perfection.
Strength training for longevity
Resistance or weight training rebuilds muscle and bone. Two or more sessions a week help preserve lean tissue, maintain insulin sensitivity, and reduce frailty [22-23].
Mind-body forms like yoga or tai chi add flexibility, balance, and calm, while also improving parasympathetic (rest-and-digest) tone [24-25].
You don’t have to lift heavy weights — body-weight exercises, resistance bands, or a few dumbbells at home can deliver real gains.
The power of combination
Programs that blend aerobic and resistance training — or include short bursts of high-intensity interval training (HIIT) — show the biggest benefits for cardiovascular health, strength, and symptom relief [26-27].
Movement also enhances mood and cognition by increasing blood flow to the brain and stimulating BDNF (a brain-growth factor).
If you’re using hormone therapy, exercise and MHT can complement each other, further improving metabolic and vascular outcomes [28-29].
Making movement realistic
Health authorities recommend 150 minutes of moderate activity weekly, plus two strength sessions [30].
But if life is busy, remember: every bit counts. Ten minutes of walking after meals, taking stairs, or dancing in the kitchen all contribute.
Find activities you genuinely enjoy — joy is the secret ingredient that turns exercise into a sustainable habit.
3. Mental Well-Being and Stress Resilience
The stress-hormone connection
Perimenopause can feel like emotional turbulence — not only because of hormones, but because midlife often carries the weight of caring for children, ageing parents, and demanding careers.
Estrogen and progesterone usually buffer the stress-response system; when they fluctuate, cortisol rises more easily [31-32]. That means the same stressors that once felt manageable can suddenly feel overwhelming.
High stress doesn’t just affect mood. It worsens hot flushes, impairs sleep, and can accelerate weight gain [33]. The good news: the brain remains plastic and trainable. You can retrain your stress response at any age.
Evidence-based mind-body tools
Cognitive-behavioural therapy (CBT), mindfulness, and acceptance-and-commitment therapy (ACT) all reduce perceived stress and improve menopausal symptoms [34-36].
Meditation and slow breathing lower adrenaline and restore calm. Even five minutes a day makes a measurable difference in heart-rate variability (your body’s stress-resilience marker).
If traditional meditation feels daunting, start with guided audios, gratitude journalling, or simply noticing five things you can see, four you can touch, three you can hear — a grounding tool that brings you back to the present.
Technology and digital support
Modern tools can help. Apps that track mood or guide meditation, wearables that monitor heart rate, and even AI-based coaching programs have all been shown to reduce anxiety and enhance motivation [37-39].
Used mindfully, they increase accountability and self-awareness — two critical ingredients for long-term change.
Mindset as medicine
Perhaps the most powerful tool of all is belief in your own ability to change. Women who approach lifestyle change with curiosity rather than criticism are far more likely to sustain it [40-41].
Remember: progress, not perfection. Every small choice that brings you calm or energy is a win for your nervous system and your hormones.

4. Avoidance of Risky Substances
What you remove matters as much as what you add
In midlife, your body’s capacity to buffer stressors like alcohol, nicotine, and recreational drugs becomes smaller. With lower estrogen and slower detoxification, even modest exposure can increase inflammation and oxidative stress [42]. Reducing or eliminating these substances gives your cells a chance to repair, hormones to rebalance, and your energy to stabilise.
Smoking
Smoking accelerates ovarian ageing, leading to menopause up to two years earlier [43]. It amplifies hot flushes, speeds bone loss, and increases cardiovascular risk by up to 40 % [44-45].
Quitting is one of the most powerful things you can do for your future health — vascular function starts to recover within months, and heart-disease risk halves within five years [46]. Some women notice small weight changes after quitting, but the metabolic and cardiovascular benefits far outweigh them [47].
Alcohol
Alcohol temporarily raises estrogen levels by increasing aromatase activity [48]. Light drinking may delay menopause slightly [49], but overall, alcohol worsens sleep, anxiety, and breast-cancer risk [50-51].
If you enjoy a drink, keep it mindful — ideally no more than one standard drink on any day and several alcohol-free days each week [52]. Notice how your body responds; many women find even small reductions improve sleep, energy, and mood.
Other substances
Cannabis, opioids, and stimulants interact with the same reward and stress circuits that shift during menopause. Women often experience stronger withdrawal and relapse vulnerability at this life stage [53]. Holistic support — combining behavioural therapy, mindfulness, and medical supervision — helps recovery while reducing stigma.
5. Restorative Sleep
When sleep falters
Sleep difficulties affect up to 60 % of women during perimenopause [54-55]. Night sweats, racing thoughts, and cortisol surges interrupt the deep, healing stages of rest. Yet sleep is when the body repairs, hormones rebalance, and the brain detoxifies.
Short sleep (under six hours) increases cardiovascular, metabolic, and mood-disorder risk [56-59]; poor-quality sleep also accelerates bone loss and cognitive decline [60-62]. You’ll likely notice that after several nights of broken rest, mood dips and food cravings rise — that’s your physiology talking.
Evidence-based support
-
Sleep hygiene: keep a consistent bedtime, avoid caffeine and alcohol late in the day, and create a cool, dark sleep space [64].
-
Mind-body tools: gentle yoga, relaxation breathing, or gratitude practice calm the sympathetic nervous system [65].
-
CBT-I: Cognitive Behavioural Therapy for Insomnia is proven to restore sleep without medication [66].
-
Exercise and daylight: morning movement reinforces your circadian rhythm [67].
-
Trackers and tech: wearables offer insight into patterns — not perfection — and can guide small improvements [68].
Remember, restorative sleep isn’t about eight flawless hours; it’s about waking feeling mentally clear and physically recharged most days.
6. Healthy Relationships and Connection
Why connection heals
Human connection is one of the most under-prescribed medicines. Strong relationships lower mortality risk by up to 50 %, a benefit equal to quitting smoking [69]. Social isolation, on the other hand, raises risks for cardiovascular disease, diabetes, and depression [70-72].
During menopause, many women feel invisible or misunderstood — yet this is precisely when belonging protects emotional and physical health.
Quality, not quantity
It’s not about how many people you know, but how supported you feel. Close, emotionally secure relationships reduce hot-flush frequency, lower stress markers, and enhance self-esteem [73-74]. Oxytocin — the “bonding hormone” — released during affectionate connection, counteracts cortisol and supports heart health [75].
Practical connection medicine
-
Reach out intentionally: join walking or hobby groups, volunteer, or reconnect with friends.
-
Communicate openly: talk with your partner about symptoms and intimacy; honesty often deepens connection [76].
-
Set boundaries: protect your energy from draining dynamics.
-
Seek community: online or local menopause groups provide validation and shared wisdom [77].
7. Premature Ovarian Insufficiency (POI)
When menopause occurs before age 40, it’s termed Premature Ovarian Insufficiency. About 4 % of women experience it [78]. Beyond fertility loss, POI increases risks for osteoporosis, cardiovascular disease, and mood disorders [79-81].
Hormone therapy is usually recommended, but lifestyle medicine is equally vital:
-
Follow a heart-healthy, Mediterranean-style diet.
-
Engage in weight-bearing exercise to preserve bone.
-
Ensure adequate calcium (1 000–1 200 mg) and vitamin D (800–1 000 IU).
-
Avoid smoking and excessive alcohol.
-
Prioritise psychological support — grief, identity, and fertility concerns are real and valid.
These steps don’t replace medical treatment, but they amplify its benefits and support emotional healing [82].

Restore Calm. Build Confidence. Gain Control.
Calm: regulate your stress system through daily movement, breathwork, and regular sleep.
Confidence: fuel your body with nutrient-rich foods and strength training that rebuilds energy and muscle.
Control: make conscious choices — reduce alcohol, stop smoking, reach out for support, and celebrate progress.
Small, consistent actions today shape the vitality, mood, and longevity of your years ahead.
Menopause is not the end — it’s the beginning of your most powerful era.
Conclusion
Menopause marks the end of reproductive years — not vitality. The research is clear: lifestyle medicine is the foundation for thriving through menopause and beyond.
When you nourish your body with real food, move daily, care for your mind, reduce harmful exposures, sleep deeply, and foster meaningful connections, you build resilience that no prescription alone can provide.
This isn’t about perfection or rigid rules; it’s about gentle consistency and self-compassion. Your midlife health story is being rewritten — and you hold the pen.
References
-
Anekwe CV et al. The Role of Lifestyle Medicine in Menopausal Health: A Review of Non-Pharmacologic Interventions. Climacteric. 2025.
-
Santoro N et al. Menopausal Transition: Mechanisms and Metabolic Implications. J Clin Endocrinol Metab. 2021.
-
Estruch R et al. Primary Prevention of Cardiovascular Disease with a Mediterranean Diet. N Engl J Med. 2018.
-
Grosso G et al. Mediterranean Diet and Menopausal Health: Systematic Review and Meta-Analysis. Nutrients. 2021.
-
Rosato V et al. Adherence to Mediterranean Diet and Mortality in Women: Cohort Analysis. Br J Nutr. 2019.
-
Kazemi M et al. Mediterranean Diet and Menopausal Symptoms: Findings from a Cross-Sectional Study. Menopause. 2020.
-
Widmer RJ et al. The Cardiometabolic Benefits of Olive Oil: Mechanisms and Evidence. Nutrients. 2019.
-
Sacks FM et al. Effects on Blood Pressure of Reduced Dietary Sodium and the DASH Diet. N Engl J Med. 2001.
-
Orlich MJ et al. Vegetarian Dietary Patterns and Mortality in Adventist Health Study 2. JAMA Intern Med. 2013.
-
Anton SD et al. Effects of Intermittent Fasting on Health Markers in Adults. Obesity. 2018.
-
Greendale GA et al. Bone Loss Over the Menopausal Transition: Results from the SWAN Study. J Bone Miner Res. 2019.
-
Ross AC et al. The 2011 Report on Dietary Reference Intakes for Calcium and Vitamin D. J Clin Endocrinol Metab. 2011.
-
Phillips SM et al. Protein Needs and Benefits in Midlife and Beyond. Front Nutr. 2023.
-
Taku K et al. Effects of Soy Isoflavone Supplementation on Menopausal Symptoms: Meta-Analysis. Menopause. 2012.
-
Frankenfeld CL et al. Equol Production and Health Implications of Isoflavone Metabolism. J Nutr. 2020.
-
Brown WJ et al. Physical Activity Patterns in Midlife Women. Med Sci Sports Exerc. 2023.
-
Rogers NH et al. Estrogen, Muscle, and Mitochondria: Mechanisms of Metabolic Protection. Endocr Rev. 2022.
-
Cornelissen VA et al. Cardiovascular Effects of Aerobic Training in Adults. Hypertension. 2013.
-
Elavsky S et al. Exercise Improves Mental Health and Physical Function in Postmenopausal Women. Health Psychol. 2012.
-
Zhang X et al. Walking Programs and Weight Outcomes in Postmenopausal Women. Menopause. 2020.
-
Moreau KL et al. Vascular Effects of Estrogen and Exercise in Aging Women. J Physiol. 2020.
-
Westcott WL et al. Resistance Training and Functional Fitness in Older Adults. Curr Sports Med Rep. 2012.
-
Villaverde-Gutierrez C et al. Exercise Interventions in Postmenopausal Women: Systematic Review. Maturitas. 2021.
-
Field T et al. Tai Chi and Yoga Effects on Physical and Mental Health. Complement Ther Med. 2013.
-
Phillips BE et al. Resistance Exercise Training and Inflammatory Cytokines. J Physiol. 2017.
-
Weston M et al. HIIT Improves Fitness and Body Composition: Meta-Analysis. Br J Sports Med. 2014.
-
Liu-Ambrose T et al. Combined Exercise and Cognitive Benefits in Older Women. J Gerontol A. 2019.
-
Pollanen E et al. Synergistic Effects of Hormone Therapy and Exercise on Metabolism. Metabolism. 2020.
-
Gupta A et al. Menopausal Hormone Therapy and Arterial Compliance. Menopause. 2022.
-
American Heart Association. Physical Activity Guidelines for Adults. 2023.
-
Parker GB et al. Neuroendocrine Links Between Stress and Depression in Midlife Women. Psychoneuroendocrinology. 2020.
-
Avis NE et al. Perceived Stress and Menopausal Symptoms: SWAN Findings. Menopause. 2015.
-
Thurston RC et al. Stress and Vasomotor Symptoms: Physiologic Pathways. Menopause. 2018.
-
Carmody J et al. Mindfulness and Menopausal Symptom Management. J Womens Health. 2019.
-
Hunter MS et al. Cognitive Behavioral Therapy for Menopausal Symptoms: Randomized Trial. Lancet. 2021.
-
Mann E et al. Relaxation Training for Hot Flushes and Anxiety in Menopause. BJOG. 2012.
-
Firth J et al. Mobile Health Interventions for Stress Reduction: Meta-Review. World Psychiatry. 2019.
-
Li Y et al. Digital Mental Health and AI-Based Chatbots in Midlife Women. Digit Health. 2024.
-
Brickwood KJ et al. Effectiveness of Wearable Fitness Trackers for Health Behavior Change. JMIR Mhealth Uhealth. 2019.
-
Bandura A. Self-Efficacy and Health Behavior Change. Health Educ Behav. 2004.
-
Pascoe MC et al. Mindfulness Meditation and Stress Hormone Regulation. Stress. 2017.
-
Anekwe CV et al. Climacteric. 2025.
-
Mishra GD et al. Smoking and Early Menopause: Longitudinal Analysis. Hum Reprod. 2021.
-
Cooper AR et al. Mechanisms of Tobacco-Induced Ovarian Damage. Reprod Toxicol. 2018.
-
Chen C et al. Smoking, Menopause, and Cardiovascular Risk: Meta-Analysis. BMJ. 2020.
-
U.S. Department of Health and Human Services. Surgeon General’s Report on Smoking and Health. 2020.
-
Anekwe CV et al. Climacteric. 2025.
-
Emanuele MA et al. Alcohol, Hormones, and the Menopausal Transition. Alcohol Health Res World. 2019.
-
Szegda KL et al. Alcohol Consumption and Menopausal Timing. Menopause. 2017.
-
Collaborative Group on Hormonal Factors in Breast Cancer. Alcohol and Breast Cancer Risk: Pooled Analysis. Lancet Oncol. 2021.
-
Zheng Y et al. Alcohol and Blood Pressure in Women: Meta-Analysis. Hypertension. 2020.
-
World Health Organization. Global Alcohol Guidelines. 2024.
-
Becker JB et al. Sex Differences in Addiction Vulnerability and Recovery. Neuropsychopharmacology. 2023.
-
Krystal AD et al. Sleep Disturbance in the Menopausal Transition. Sleep Med Clin. 2020.
-
Baker FC et al. Sleep Quality and Hormonal Changes in Midlife Women. J Clin Endocrinol Metab. 2018.
-
Cappuccio FP et al. Sleep Duration and Cardiovascular Mortality: Meta-Analysis. Eur Heart J. 2011.
-
Javaheri S et al. Sleep and Heart Disease Risk in Women. Circulation. 2020.
-
Pase MP et al. Sleep Duration and Cognitive Decline. Sleep. 2019.
-
WHI Investigators. Sleep Duration and Coronary Events in Women. J Am Heart Assoc. 2022.
-
Reid KJ et al. Sleep Fragmentation and Bone Density. Sleep Health. 2021.
-
Greendale GA et al. Sleep and Cognitive Function in the SWAN Cohort. Neurology. 2010.
-
Zheng H et al. Insomnia and Depression During the Menopausal Transition. Sleep Med. 2021.
-
Baglioni C et al. Bidirectional Relationship Between Insomnia and Depression. J Affect Disord. 2020.
-
Irish LA et al. Sleep Hygiene and Behavioral Interventions. Sleep Health. 2015.
-
Rusch HL et al. Yoga and Meditation for Sleep Improvement. Front Psychol. 2019.
-
Kuhn E et al. Cognitive Behavioral Therapy for Insomnia in Midlife Women. Sleep. 2022.
-
Buman MP et al. Physical Activity Timing and Circadian Rhythm. Sleep. 2020.
-
Lee SY et al. Accuracy of Consumer Sleep-Tracking Devices. Sensors. 2023.
-
Holt-Lunstad J et al. Social Relationships and Mortality Risk: Meta-Analysis. PLoS Med. 2010.
-
Steptoe A et al. Loneliness and Physical Health Outcomes. Nat Hum Behav. 2020.
-
Vogt T et al. Social Isolation, Inflammation, and Cardiometabolic Health. J Gerontol B. 2021.
-
Cacioppo JT et al. Loneliness and Health: Biological Mechanisms. Perspect Psychol Sci. 2015.
-
Avis NE et al. Social Support, Relationship Quality, and Menopausal Symptoms. Menopause. 2019.
-
Kim HJ et al. Social Support and Bone Health in Postmenopausal Women. Osteoporos Int. 2018.
-
Heinrichs M et al. Oxytocin, Trust, and Stress Regulation. Biol Psychiatry. 2009.
-
Kingsberg SA et al. Communication and Sexual Health in Menopause. Sex Med Rev. 2021.
-
Martinez M et al. Online Peer Support for Menopausal Women: Qualitative Findings. J Womens Health. 2023.
-
Golezar S et al. Global Estimates of Premature Ovarian Insufficiency Prevalence. Hum Reprod Update. 2020.
-
Anderson RA et al. Cardiovascular and Bone Risks in Premature Ovarian Insufficiency. Hum Reprod Open. 2024.
-
Daan NM et al. Hormonal and Metabolic Sequelae of Premature Ovarian Insufficiency. J Clin Endocrinol Metab. 2021.
-
Faubion SS et al. Mood Disorders and Quality of Life in Women with POI. Menopause. 2020.
-
ESHRE/ASRM/IMS. Guideline on Management of Premature Ovarian Insufficiency. 2025.
Want my best free resources
Pop your name in and I will send you to my VIP resource page- more great gut tips included.
We hate SPAM. We will never sell your information, for any reason.





